Counselors - Peers - Marriage and Family Therapists - Addiction Counselors
Psychologists - Social Workers - Pre-licensure Professionals - Interns
...for a diverse, competent, and sustainable behavioral healthcare workforce.
- Home
- Timeline
Active Concerns (2023)
| Concern | Proposal | Since When |
|---|---|---|
| Commercial lease restrictions on therapy offices | Colorado shall prohibit commercial landlords from restricting commercial spaces to a single mental health office. "Non-compete" rules are more appropriate for retail and limit client access to care. | 2024 |
| MHPAEA Parity Enforcement | As other states have done, since the federal government (CMS) has signaled no interest in pursuing state departments' Medicaid Parity violations, Colorado requires a Parity enforcement mechanism to hear, substantiate and consequence MHPAEA Parity violation. This could be through the Behavioral Health ombuds office, the Attorney General, BHA, or other independent agency that can evaluate Parity violation claims. | 2019 |
| Supervised services in commercial contracts | Medicaid disenrollment (May 2023 extending into 2024 for twelve or more months) will reduce Colorado Medicaid from 1.7 million Coloradans to around 1.1 million. Some of those leaving Medicaid due to higher income will purchase ACA subsidized plans on the Health Exchange. These plans are managed by commercial insurance payers, who may or may not allow supervised services by pre-licensure clinicians under supervision. COMBINE seeks uniformity and allowance for pre-licensure work for both MA graduates and university interns. | 2023 |
| Reimbursement rate stability (Parity) | The rate setting process for medical care is substantially different from that process for mental health care, which violates MHPAEA Parity. | 2019 |
| Inaccurate Network Adequacy reporting | HCPF requires RAEs (Managed Care Entities) to provide network reports quarterly. HCPF is also required to post reports quarterly, publically. Neither RAEs nor HCPF count or report the candidate counselors or university interns that provide care. There is no accurate number that helps understand the capacity of the workforce. A modifier code indicating that the service was actually rendered by a supervised counselor or NPI numbers for pre-licensure staff would help. | 2020 |
| Legislative Oversight | The Colorado legislature holds SMART Act hearings annually. These have devolved into departments offering summary reports of activity with no challenge to the statistics presented. | 2020 |
| Long RAE contracting times | Unlike medical providers, who are ready to work after HCPF "validation," mental health providers must take additional steps, which are contracting with managed care entities (RAEs). RAEs often take longer than the 90 days specified in HCPF - RAE contracts to actually contract. Additionally physicians are privileged by a law requiring commercial payers contract within 60 days. | 2021 |
| Behavioral Health Entity licensing | COMBINE cooperates with the BHA Behavioral Health Authority to create and support rules that make sense for increasing quality of service and safety. Many of our small and solo clinics need appropriate waivers for building zoning and construction codes, and for supervision ratios for university interns and pre-licensure candidates. | 2023 |
| Audit of managed care entities | COMBINE continues to advocate for oversight of the manages care entities. Colorado policy makers and tax payers cannot get even basic information like network capacity and results of care coordination efforts. | 2020 |
| CCAR exemption | The CCAR is an extensive and intrusive survey that was dropped for outpatient Medicaid providers in 2018. The BHA has proposed that outpatient care must participate in the CCAR program. No action is taken based on collected CCAR data, so COMBINE's position is that data from claim forms is sufficient. | 2023 |
| Z code requirements for children | While COMBINE supports gathering actionable data, requiring Z-codes on child Medicaid service claims yields nothing reliable or valid, as many children will be assessed as meeting criteria for many Z-codes. Providers will variably assess children leading to noisy data. | 2023 |
| Exclusion of mental health care from eConsult | HCPF funded a large project enabling communication between health care providers, yet excluded mental health care. | 2022 |
| Support Colorado's Behavioral Health Ombuds Office | The Ombuds office for Behavioral Health is understaffed for the task it's mandated to do. | 2023 |
Timeline, Related Documents, and Released Documents from COMBINE
| Feb 24 2024 | Feb 2024 Parity Comments for HCPF | COMBINE published 2024 Parity Comment in response to HCPF's annual call for comments. | |
| Feb 1 2024 | 2024 Senate Bill 93 Continuity of Care | COMBINE took an amend position on SB24-093, which allows for continuity of care when a person moves from Medicaid to another insurance. Mental health care was not included in the draft. | |
| Dec 1 2023 | COMBINE requests an open meetings policy from HCPF after public online meetings no longer display participants. | ||
| November 28 2023 | COMBINE seeks clarity from CHP+ managers regarding supervised billing. | ||
| COMBINE requests HCPF policy regarding stakeholder meetings after an HCPF "stakeholder" meeting (regarding requiring a Z-code for children as a diagnosis) where no participants could see the other participants and Q&A was hidden. | |||
| November 8 2023 | | COMBINE clinic directors file complaints with Division of Insurance to seek compliance by UnitedHealth (RAE 1, commercial) with DOI directive to allow supervisory billing. | |
| November 3 2023 | | Action: Ask Legislators to support BHOCO with 10 FTE. | |
| October 20 2023 | HCPF HB 23-1269 Directed Payment Legislative Report | HCPF releases HB23-1269 mandated report related to minimum rates. This is a very important document as HCPF admits that it has the power to mandate minimum rates from RAEs. | |
| October 20 2023 | HCPF proposes requiring Z-codes to gather SDOH (social determinates of health) data for children under 21 years old, contrary to law. | ||
| October 19 2023 |
Tue, May 17, 2022, 3:37 PM Thanks for reaching out. The statewide Medicaid eConsult platform will not include behavioral health as part of its specialty services, however we are hopeful that we will be able to explore and potentially provide this service at a later date. Please continue to send us your feedback and any questions that come up overtime. Thanks and have a great afternoon, eConsult Development Team | HCPF continues to exclude mental health care from the eConsult system, which allows PHI (protected health information) to be communicated between primary care physicians and specialists. CMS stated that care coordination between medical providers and mental health providers increases quality of care and decreases overall health care spending. COMBINE alerted HCPF to this Parity concern in 2022. | |
| October 12 2023 | Requesting RAE audit by LAC 2023 |
Since 2019, COMBINE has advocated for more oversight of the Medicaid mental health care managers, the "RAEs", who are actually Anthem, United Healthcare, and Access Management (Colorado Access) The Legislative Audit Committee controls the work of the Office of State Auditors, who are empowered to audit state departments and agencies. For the OSA to audit RAEs, they need additional power. | |
| October 11 2023 | CCAR BHA comment.pdf | COMBINE advocates for exemption from CCAR data recording requirements for non-SUD outpatient care. | |
| August 30 2023 | Regarding BHE Licensing | COMBINE advocated for reasonable rules for licensure of small mental health clinics, including waivers for Certificate of Compliance from Dept of Fire Prevention and Control, training requirements, medical assessments, and referring agency relationships. | |
| August 1 2023 | HCPF 22-1268 Action Plan | HCPF admits it has the power to set minimum rates and explains that it has already done so for some services. HCPF discusses direct payments to support the independent providers. HCPF forwards a narrative that comparing Medicaid rates to "commercial rates" is proper, rather than Medicare rates, neighboring states' rates, private market rates, or rates that will increase the network size. | |
| June 6 2023 | B-4.131 Policy Directives for Credentialing Standards and Timeline for Mental Health, Behavioral Health, and Substance Use Disorder Providers | COMBINE received support from Colorado's Division of Insurance in regards to commercial payers not allowing supervised services. | |
| Feb 28 2023 | BHA Rules comment on Behavioral Health Entity licensing and requirements | COMBINE joined with other providers in a collaborative effort with the Behavioral Health Administration for reasonable licensing and regulation of small clinics. Proposed rules would have closed nearly all small clinics with internship programs. | |
| Dec 9 2022 | RAE 3,5 (Colorado Access/Access Management) switched direct deposit vendor, which demands a 2% fee on direct deposits. Creates administrative hassle for clinics. Eventually offers a no-fee option. | ||
| Dec 4 2022 | RAE 6,7 (CCHA/Anthem/Carelon) fails to pay claims for weeks. | ||
| Sept 29 2022 | LAC committee audio recording. | Colorado's LAC drops expansion of OSA authority to audit RAEs. OSA is the Office of State Auditors, which is controlled by the LAC, the Legislative Audit Committee. Rep. Michaelson Jenet stated, "lets see what the BHA is going to do." RAEs are not government agencies so expanding audit power would be significant and is therefore problematic. | |
| Sept 23 2022 | COMBINE Memo to Legislators re RAE Supervised Practice Policy | "Both of these proposed changes will impact the workforce, reducing opportunities for early career counselors to receive supervision, and prohibiting qualified professionals from working." | |
| Sept 10 2022 | Regarding RAE Supervised Practice Policy |
Kimberly M. Muhlebruch, Clinical & Executive Supervisor, SOBT Therapy, LLC; Centennial discusses necessity for supervision of early career therapists in diverse workplaces. |
|
| Sept 9 2022 | Letter to legislators regarding Supervision Policy from US Army veteran and clinic owner |
"I am worried, no terrified, that they will decide to implement this new rule and that small businesses like my veteran owned counseling practice will be shut down." | |
| Sept 5 2022 | COMBINE Response to HB22-1268 Report |
"The report: ● Meets neither the letter nor the spirit of the law, which was, to contract with an independent auditor to both review and remedy the inequitable payment models existing currently, ● ignores the impact these inequitable rates impose on the workforce at Centers, ● maintains a vague and incomplete narrative about the rate setting process, ● obfuscates the corporate capture of the state’s $1 billion Medicaid mental healthcare system, ● minimizes the work of the IPN and ignores the cost of that work, ● does not discuss MHPAEA Parity concepts relating to rates, ● minimizes the rate differences, ● does not provide context for important statistics, ● does not offer adequate recommendations to remedy the enormous payment variation, ● offers “value based payments” as the remedy to rate differences, and ● confuses the workforce, the public, and the legislators. |
|
| August 20 2022 | HB 22-1268 Report |
This "BEHAVIORAL HEALTH PROVIDER RATE COMPARISON REPORT" was mandated by legislation, with the purpose of explaining why independent providers are paid 1/5 of the rate that Community Mental Health Centers are paid for the same 55 minute outpatient psychotherapy sessions. The report was produced by "independent auditors, CBIZ Optumas (DBA Optumas; formerly Schramm Health Partners LLC) and Myers and Stauffer." |
|
| July 2022 | COMBINE Policy Asks 2022 | (with strike throughs for resolved issues). Enumerates top concerns, HCPF clarifications, DORA and OBH concerns, early childhood and workforce pipeline, DEI, Parity, ethics concerns, and long term goals. | |
| July 20 2022 | Response 2022 HCPF Parity "Report" | HCPF in 2022 continued to obfuscate and deny that the RAE structure itself is an MHPAEA Parity violation, ignoring the significant differences in rate setting policy between medical/surgical and behavioral health. | |
| July 7 2022 | COMBINE forms a 501c4 Trade Association (COMBINE Action), increases dues, and reports over 150 members. Board Chair Yakitta Renfroe Board Members: Carlos Villafan, Faith Halverson Ramos, Lexi Ellis, Andy Rose | ||
| ' June 2 2022 | ... tired of being judged by White therapists... | "We have heard time-and-time again from our BIPOC population that they were tired of being judged by White therapists, or stereotypes/assumptions by someone who claimed to be “woke” or in need of being a “white savior” or misunderstanding the trauma related to police brutality and the fear of being a population that no one cared about. It is microaggressions such as those statements that either pushed the BIPOC population away from therapy or encouraged them to have a louder voice to advocate for someone that knew them on a level that they did not have to explain." | |
| March 2022 | COMBINE and Colorado Access cooperate on a pilot program for allowing pre-licensure supervised care, after two years of Colorado Access prohibiting the practice. All other RAEs allowed this. | ||
| February 2022 | Senate Health Committee remarks on prior authorization | Colorado legislators introduced protections on prior authorization in the 2022 session. Eventually these policies were moot as SB 22-156 rules out prior authorization for Medicaid outpatient mental health care. | |
| January 2022 | Behavioral Health Workforce is a National Crisis | (3rd party document) Health Management Associates and National Council for Mental Wellbeing. Discusses: policy, funding, administrative burden, GME (graduate medical education) for behavioral health, and some state strategies. | |
| Dec 15 2021 | JBC 2021 HCPF Number of Providers.pdf | HCPF presented statistic to the Joint Budget Committee and COMBINE responded with concerns about those statistics. The actual strength of the workforce was not tracked, as neither HCPF nor RAEs took interest in the amount of pre-licensure work being delivered. | |
| November 18 2021 | Dr. Griffiths Letter of Concern Nov 2021 | Extensive details of RAE challenges and goals for the workforce. Includes: credentialing, attribution, access to care, prior authorization, RAE specifics, psychological testing, Parity, rates, no-show fees, and a summary. | |
| April 1 2021 | COMBINE Parity Concerns submitted for HCPF Parity Report | HCPF asks for Parity concerns, COMBINE provides comments related to: Parity requirements in RAE contracts, Parity law covers Colorado Medicaid, reimbursement, prior authorization, NQTLs, restrictions by Colorado Access on pre-licensure service, member attribution, network adequacy, credentialing, care guidelines, medication management, payer mix, extension codes, governance, and Parity enforcement. | |
| March 6 2021 | Colorado Access Dr. Bremer Letter | COMBINE letter to Colorado Access requesting coverage for pre-licensure services, as other RAEs were allowing. Co-signed by clinic directors. | |
| March 5 2021 | DORA Board of LPC Examiners met Friday, March 5. The Board approved Naropa University’s application for CACREP equivalency for the class of 2021. So that current 3rd year students could apply for their LPCC before graduation. | ||
| March 2021 | 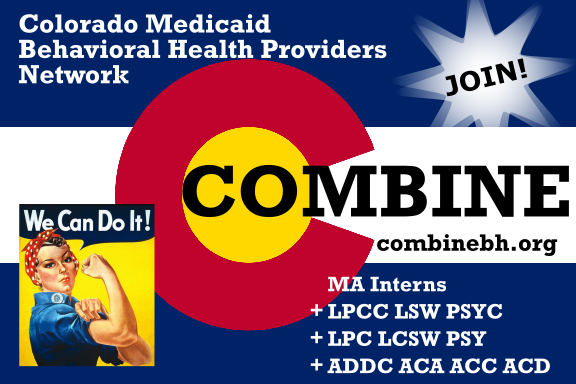 | COMBINE gets graphics. | |
| March 1 2021 - August 2021 | Anthem introduced Prior Authorization for routine outpatient care, in violation of Parity. COMBINE supported clinicians in complying and also advocated for an end to this burdensome and unnecessary practice. Anthem abandoned this policy in August of 2021 after intense advocacy. | ||
| March 31 2021 | HCPF Rate Review Questions | Clinic directors respond to HCPF request for information about how RAEs are operating. | |
| March 1, 2021 | SB 126 Contracting Time Leg Letter | Legislation (SB21-126) was introduced to limit contracting time to 60 days, but mental health care workers were left out of the legislation. COMBINE sent letters to sponsors. | |
| March 1 2021 | Prior Auth Client Letter English.pdf | Anthem (RAE 6,7 Boulder/ Golden/ CO Springs) introduced a Prior Authorization requirement. COMBINE advocated against this administrative burden and collected evidence that most, and for some clinics, all prior authorizations were approved. Anthem dropped the policy in September of 2021. This letter was to inform our clients about the change, and how it would impact their care, and who to reach out to to take a stand. | |
| Feb 28 2021 |
|
Reviews MHPAEA Parity concerns : depression screening, complete mental health screening, court ordered services are covered, underlying causes, prior authorization, extension codes, supervised work. | |
| Feb 21 2021 | Oversight Questions for the Joint Budget Committee | COMBINE sends oversight questions for the Joint Budget Committee for their HCPF hearing. Topics: network adequacy, reimbursement, MHPAEA Parity, prior authorizations, and credentialing. | |
| Feb 15 2021 | COMBINE review of Network Adequacy Reports | RAEs submit data to HCPF quarterly regarding their provider nettworks. HCPF is obligated to produce network adequacy documents for the public. These reports are examined in this document. Of concern: provider-member ratios, delayed data, missing data, late reports, incorrect dates, how providers are counted, lack of data about pre-licensure services, inclusion of "other counties", varying baselines, and large redactions. | |
| Jan 16 2021 | COMBINE Facebook group was established and an Action email list was established with "9 subscribers and 8 dues paying voting members." Also published: Response to HCPF's answers to the Joint Budget Committee where we see the pattern of obscuring the RAEs and their policies. COMBINE engaged with Colorado Access because they were prohibiting pre-licensure work by supervised candidates and university interns, contrary to the other RAE's policies. Colorado Access was only allowing supervised service where there's a facility license, which was a substantial barrier to entry. | ||
| Dec 29 2020 |  | COMBINE forms a Small Donor Political Committee to contribute to political campaigns. | |
| Jan 5 2020 | Letter To Editor: Protect mental health safety net | This letter appeared in Boulder Beat, a local news outlet in Boulder County. | |
| Nov 19 2019 | Boulder City Council contemporaneous tweets | Shay Castle of Boulder Beat tweeted out this city council meeting where COMBINE organized with Colorado Counseling Association (Ryan Burkhart) to request legislative lobbying help from Boulder's lobbyists to protect Medicaid mental health care, following the 20% cut. | |
| November 2019 | Appeal to Hufford w Pogar Notes, Singer Agenda.pdf | COMBINE intially organized to challenge a 20% cut to reimbursement rates for outpatient Medicaid mental health service providers, who had been contracted by Medicaid managers. Anthem (RAE 6,7) had paid the MPRRAC rate in 2018 and 2019 and then explained that they had "made a mistake." This document shows an appeal by Andrew Rose to Brian Hufford, a lawyer on the landmark Witt v United Healthcare Parity case. Rose and his wife Sarah met with Anthem representatives Janet Pogar and Erica Kloehn and this document contains contemporaneous notes of that meeting, which was unproductive. State Representative Singer (D-Longmont, Chair of the Colorado House's Public & Behavioral Health & Human Services ) also met with Rose and HCPF to discuss the rate cut. Melissa Eddleman represented HCPF in that meeting, which was unproductive. HCPF's position was that rates were not their business and RAEs could do what they wanted to. This document has a meeting agenda. |
